A Practical Guide to Recovering from a Nervous Breakdown in the UK
- Therapy-with-Ben
- Dec 12, 2025
- 17 min read
Authored by: Therapy-with-Ben
The journey back from a mental health crisis, what many of us call a nervous breakdown, is a gradual one. It's not a race. The process hinges on getting to a safe place, finding the right support, and gently rebuilding routines that actually work for you. The very first thing to do is secure your environment and call someone you trust or a crisis service. This creates a small island of stability, a safe base from which you can start to heal.
Your First Steps After a Mental Health Crisis
The moments just after a mental health crisis can feel utterly disorienting, even terrifying. It's so important to hear this: what you've just been through is not a sign of weakness. Far from it. Think of it as your mind and body's final, desperate signal that the stress you've been under is simply too much. It's a sign that something has to change.
Recovering doesn't start with big, dramatic life changes. It begins with small, deliberate steps designed to bring back a sense of safety and calm. In these first 24 to 48 hours, your only job is to stabilise. Forget about solving the bigger picture for now. Just focus on the here and now.
Finding a Safe Space
Your absolute first priority is to get somewhere you feel physically and emotionally secure. That might not be your own home, and that’s okay, especially if it’s a source of stress. Perhaps it’s a good friend’s house, a family member’s quiet spare room, or anywhere you can just be, without pressure.
The goal is to dial down the noise, both external and internal. Mute your phone notifications. Dim the lights. Give yourself permission to do absolutely nothing but breathe. This isn't about avoiding your problems; it's a vital act of self-preservation. You're giving your nervous system the chance to come down from high alert.
Reaching Out for Immediate Support
You really don't have to go through this on your own. In fact, feeling isolated can make everything feel a hundred times worse. Reaching out to someone is a huge, critical step. It could be your partner, a close mate, or a family member who you know is a good listener and won't judge.
All you need to say is, "I'm not okay and I need some help." You don't need to have all the answers or a neat explanation. The point is to let someone in, to have another person's voice on the phone or their presence in the room act as an anchor in the storm.
This simple flow—Secure, Support, Services—is the core of crisis response. It all starts with safety and connection.
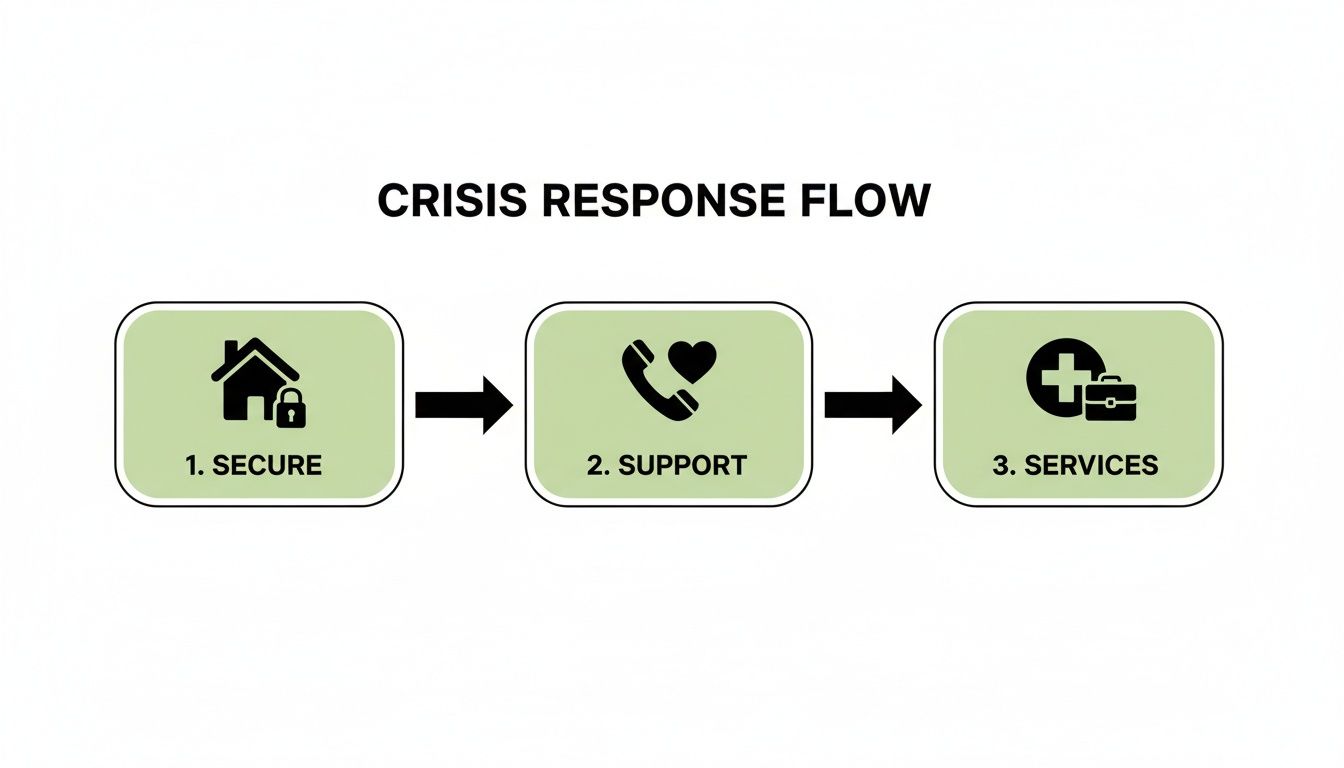
This process really highlights that your first moves should always be grounded in getting safe and making contact before you even think about formal help.
When to Contact UK Crisis Services
Sometimes, the support of friends or family isn't available, or it might not feel like enough. This is exactly what UK crisis services are for. They are staffed by trained professionals ready to offer immediate, confidential support when you feel you have nowhere else to turn.
If you are feeling desperate, unsafe, or at risk, please consider these options.
In a crisis, having a clear plan can cut through the panic. The table below is a quick-reference guide for those first critical hours.
Immediate Crisis Action Plan
Priority Action | Why It Is Important | UK Contact / Resource |
|---|---|---|
Call 999 | If you or someone else is in immediate danger or at risk of harm. | Call 999 for emergency services. |
Contact NHS 111 (Option 2) | For urgent mental health advice and connection to local NHS support teams. | Call 111 and select the mental health option. |
Talk to The Samaritans | They provide a non-judgemental listening ear, 24/7. | Call 116 123 for free, anytime. |
Text 'SHOUT' | If talking feels impossible, this text service offers silent, in-the-moment support. | Text 'SHOUT' to 85258. |
Find a Safe Place | Removes you from immediate stressors and allows your nervous system to calm down. | A trusted friend's home, a quiet room, or anywhere you feel secure. |
This isn't an exhaustive list, but it's a solid starting point for taking control when everything feels like it's spiralling.
A nervous breakdown is your system's final, desperate attempt to get your attention. Your first act of recovery is to listen to it by prioritising safety and rest above all else.
This initial period is all about giving yourself the compassion and space you so desperately need. By taking these first few steps, you're laying a solid foundation for the healing journey that lies ahead. For a wider look at available support, you might find this guide on essential mental health resources for everyday needs helpful.
Understanding What Led to Your Breakdown

Once you’ve found a safe space, the journey back to yourself begins with a bit of gentle exploration. It’s so important to realise that what you’ve experienced isn’t a sign of failure. Far from it. A breakdown is often the body’s final, desperate signal after being pushed far beyond its limits for too long.
This isn't about blaming yourself or getting lost in regrets. It’s about gently and compassionately untangling the different threads that led you here. When you start to see the causes clearly, you can begin to address them properly, and that’s the real foundation for a lasting recovery.
The Anatomy of Overwhelm
A mental health crisis doesn't just appear out of the blue. It’s almost always the end result of immense, sustained pressure. Think of it as a reservoir slowly filling up; individual stressors might seem manageable on their own, but together, they build until one final drop of rain causes the dam to break.
That final trigger can often feel confusingly small or insignificant. But it’s the chronic, underlying stress that’s done the real damage. Grasping this can help quieten that voice of self-blame that so often pipes up when we’re at our most vulnerable.
Common Triggers and Real-World Scenarios
While everyone's story is unique, the sources of chronic stress often fall into familiar patterns. Sometimes, seeing your own experience reflected in someone else’s can be a huge relief, a quiet reminder that you're not going through this alone.
Here are a few anonymised stories drawn from real-life experiences I've encountered:
Relentless Workplace Pressure: "Sarah," a project manager, had been pulling 12-hour days for months to hit a critical deadline. The constant ping of emails after hours, the pressure from above, and the fear of things going wrong slowly chipped away at her. One morning, she found she simply couldn't bring herself to open her laptop.
Profound Personal Challenges: "David" was juggling a full-time job and his own young family while also being the main carer for his elderly mother. The emotional toll, the financial strain, and the complete lack of time for himself just built and built, until he started having intense panic attacks and feeling emotionally numb.
Significant Life Changes: After a painful divorce, "Chloe" felt completely lost. The grief, piled on top of the stress of finding a new place to live and managing money on her own, left her so drained that even small decisions felt impossible. This paralysis eventually spiralled into a crisis.
These examples show how different parts of our lives—work, family, and personal upheaval—can become sources of overwhelming stress. Your own story will have its own details, but that pattern of escalating pressure is something many people will recognise.
At its heart, a breakdown is often about the gap between the demands placed on you and the resources you have to cope. Recovery begins when you start to close that gap—either by reducing the demands or by rebuilding your resources.
If any of these stories resonate, it’s a good sign that you've been carrying far, far too much for far too long.
You Are Not Alone in This Struggle
It’s easy to feel completely isolated in this, but struggling with severe stress is an incredibly common experience here in the UK. The demands of modern life, financial worries, and what we feel is expected of us are taking a real toll on our collective mental health. National surveys have shown a worrying trend in our overall wellbeing.
For example, a recent report from Mental Health UK revealed that a staggering 91% of adults felt high or moderate stress in the last year. Data from the Office for National Statistics also showed that 18% of adults were experiencing moderate to severe depressive symptoms during one survey period. These aren't just numbers; they represent real people struggling, especially younger people, with around 35% of 18–24 year‑olds taking time off work for stress-related poor mental health. You can read more about these UK mental health findings and their context.
Realising you’re part of a much bigger picture can help lift the weight of personal failure. It reframes what’s happened not as your fault, but as a deeply human response to an increasingly demanding world. Understanding the 'why' is the first powerful step you can take towards healing.
Navigating Professional Support in the UK
Taking that first step towards professional help is often the hardest, but it's a monumental sign of strength. It's you saying, "I can't carry all this on my own anymore," and that's a huge moment in any recovery.
But let's be honest, figuring out how to get that help in the UK can feel like a maze, especially when you're already feeling fragile and overwhelmed. This is your practical map to cut through the confusion. We'll walk through the main routes for support, from the NHS to private options, so you can feel more in control.
Starting with Your GP
For most of us, the journey starts at our local GP surgery. Your doctor is a key ally here. They are your first port of call to listen, assess what's going on, and point you towards more specialised services. They can also discuss whether medication might be part of the picture for you.
A good tip is to book a double appointment if you can. Before you go, jot down a few bullet points on your phone or a bit of paper: what are your main symptoms? How long has this been going on? How is it messing with your day-to-day life? Having these notes helps you stay on track and makes sure you don't forget something vital when you're feeling the pressure. You don’t need a perfect speech prepared—just being honest is more than enough.
NHS Talking Therapies
One of the most common pathways your GP will suggest is a referral to your local NHS Talking Therapies service (you might still hear it called IAPT). These services are designed to offer proven therapies, mostly Cognitive Behavioural Therapy (CBT), for issues like anxiety and depression, which are often at the root of a breakdown.
The good news is that in many areas, you can now self-refer online without needing to see a GP first, which can speed things up.
The process usually kicks off with an assessment, often over the phone, to see what kind of support fits your needs. While the NHS is an incredible resource, it's useful to have a realistic view. Recent data shows that 91.2% of people were seen within six weeks, which is great. However, the same report found that only 46.8% of patients reached what's called "reliable recovery." You can explore more about NHS therapy access and outcomes here.
This just shows that while NHS Talking Therapies can be a fantastic starting point, for many, it’s just one part of a much longer journey that might require different or more sustained support.
Exploring Private and Specialised Therapy
The NHS provides a vital service, but it's not always the perfect fit for everyone. Waiting lists for specific types of therapy can be long, and the approach on offer might not be what you feel you need. This is where looking at other options can make a real difference.
Going private opens up a much bigger world of therapists and therapeutic styles, like psychodynamic or person-centred counselling. It also means you can usually get started much, much faster. The main hurdle, of course, is the cost, but don't let that stop you from looking. Many therapists offer sliding-scale fees based on income or have cheaper introductory sessions.
It’s also worth seeking out specialised approaches that feel right for you. For example, in my own Cheltenham practice, I offer walk-and-talk therapy. It combines a counselling session with gentle movement out in nature. For a lot of people, not having to sit face-to-face in a quiet room makes it so much easier to open up and process tough feelings.
Comparing Your Options
So, what’s the right path for you? It really comes down to your personal situation – what you need, what your budget is, and how quickly you need support.
To help you get a clearer picture, here's a quick comparison of the main routes available in the UK.
Comparing Therapy Options for Recovery
Therapy Type | Best For... | Typical UK Wait Times | Potential Cost |
|---|---|---|---|
NHS Talking Therapies | Initial support for common issues like anxiety & depression, primarily with CBT. | A few weeks to a few months. | Free |
Private Counselling | A wider choice of therapy types, faster access, and longer-term support. | A few days to a couple of weeks. | £50 - £120+ per session |
Charity/Low-Cost Services | Affordable, accessible therapy for those on a low income. | Can be long; varies by charity. | Free, donation-based, or low-cost |
Specialised Therapy | Specific needs, like trauma therapy, or unique approaches like walk-and-talk. | Varies, but often faster than NHS. | £60 - £150+ per session |
Ultimately, choosing a path is less about finding the "best" one on paper and more about finding what works for you right now.
The "best" type of therapy is the one that you can access and that feels right for you. Trust your instincts when speaking to potential therapists; the connection you feel with them is one of the most significant factors in a successful outcome.
Understanding this landscape is the first step. Whether you go through the NHS, find a private counsellor, or try a local service, getting professional support gives you a safe, non-judgemental space where you can finally start to heal and rebuild.
Building Your Personal Recovery Toolkit
While getting professional support is a massive step forward, it’s the small, consistent things you do every day that really build lasting wellbeing. Recovering from a breakdown isn't about grand, sweeping gestures. It’s about creating a personal toolkit of strategies that ground you, calm your system, and slowly build back your resilience from the inside out.
Think of it as a collection of go-to habits and resources for when you feel overwhelmed, exhausted, or just a bit lost. The aim is to build a foundation so solid that it supports you not just now, but for years to come.
The Foundational Pillars of Mental Health
When your whole system is running on empty, the basics matter more than ever. Sleep, nutrition, and gentle movement are the three pillars that hold everything else up. Trying to dive into complex self-care without sorting these first is like trying to build a house on sand.
But please, be gentle with yourself. Your energy is probably at an all-time low, so the key is to start incredibly small.
Sleep: Forget striving for a perfect eight hours straight away. That’s too much pressure. Instead, just focus on creating a simple 'wind-down' ritual. This could be as easy as dimming the lights an hour before bed, putting on some calming music, or sipping a caffeine-free tea.
Nutrition: Cooking can feel like climbing a mountain when you’re exhausted. Don't beat yourself up about preparing elaborate meals. Just focus on nourishment, however you can get it. Can you add a handful of spinach to a ready-made soup? Or have a piece of fruit with your toast? These small upgrades make a real difference.
Gentle Movement: This is not the time for intense exercise. The real goal is to reconnect with your body in a kind, gentle way. A five-minute walk around the block, a few simple stretches first thing in the morning, or even just standing outside for a moment can help shift your energy. You can discover more about the profound mental health benefits of nature in our related article.
These small, consistent efforts are what help regulate your nervous system, giving you a stable base from which you can start to properly heal.
Practical Tools for an Overwhelmed Mind
Once those foundations feel a little more stable, you can start adding more specific tools to your kit. These are techniques designed to help you manage intrusive thoughts, process difficult feelings, and bring a sense of calm when your mind feels like a whirlwind.
One of the most powerful tools I’ve seen work for clients is journaling. It’s a simple way to get all those swirling, stressful thoughts out of your head and onto paper, where they somehow seem much more manageable. You don't need to write pages and pages; a few bullet points can be just as effective.
Your recovery toolkit is deeply personal. What works for one person may not work for another. The goal is to experiment with kindness and curiosity, keeping what serves you and letting go of what doesn't.
If you’re stuck, here are a few prompts to get you started:
What is one small thing I can realistically do for myself today?
What emotion am I feeling most strongly right now, and where do I feel it in my body?
Write down three things you can see, two things you can hear, and one thing you can feel.
Mindfulness is another crucial skill. It’s simply the practice of paying attention to the present moment without judgement. A wonderfully simple technique is the 3-3-3 rule: when anxiety starts to rise, just pause and name three things you can see and three sounds you can hear. Then, move three parts of your body. This simple action pulls you out of the storm in your head and back into the present moment.
Setting Boundaries and Creating Comfort
A huge part of recovering from a breakdown is learning how to protect your energy. This means setting firm but compassionate boundaries with people, work, and even your own inner critic.
Saying "no" isn't selfish; it's a vital act of self-preservation right now. Start small. Decline a minor request you don’t have the energy for, or schedule a non-negotiable hour of quiet rest into your day.
Creating physical comfort is also a surprisingly powerful tool. This could mean investing in a really soft blanket or some comfortable clothes. As you build your toolkit, you might explore things designed to soothe the nervous system; you can even find local resources for anxiety blankets. The key is to create a safe, comforting environment that sends a clear signal to your body that it’s okay to relax.
Authored by: Therapy-with-Ben
Rebuilding Your Life and Preventing Relapse
True recovery isn’t about rewinding the clock and getting back to the exact life you had before. Let's be honest, in many ways, that life is what led you here. The real work is about consciously building a new life—one that’s more sustainable, authentic, and genuinely supportive of your wellbeing.
This is the long-term journey, the part where you learn to prevent a relapse.

It involves practical steps, like figuring out work and reconnecting with people, but the core of it is a deeper commitment to yourself. You'll start listening to your body's early warnings and create a plan that puts your mental health first. Always.
Managing a Return to Work
Heading back to work can feel like a huge milestone, but it often brings a knot of anxiety with it. The key is to manage it on your terms. Jumping back into the deep end isn't the goal; your health is the priority.
A phased return is often the wisest approach. This could mean starting with shorter hours or fewer days a week, giving you space to gradually build up your stamina and confidence.
It's also worth knowing that under UK law, your employer has a duty to make reasonable adjustments for your mental health. Don’t be afraid to ask for what you need. This could look like:
Temporarily reducing your workload or specific high-pressure tasks.
Allowing for more flexible hours or some remote work.
Setting up regular, informal check-ins with your manager to see how you're coping.
Approaching this conversation with a calm, clear plan can make all the difference. You don't need to share every detail. Simply explaining that you are recovering from a period of ill-health and that these adjustments will support a successful return is enough.
Repairing and Reconnecting Relationships
A mental health crisis can put an immense strain on your relationships. Friends, family, and partners likely felt worried, confused, or maybe even hurt. As you heal, you can begin to mend these connections, but it requires patience and open communication from both sides.
Start by explaining what happened in a way that feels comfortable for you. It could be as simple as, "I was dealing with an overwhelming amount of stress, and my system just shut down. I’m learning how to manage things differently now."
Rebuilding that trust and connection takes time. Focus on small, positive interactions rather than aiming for one big, problem-solving conversation. Suggest a quiet coffee or a short walk. It’s about showing, through your actions, that you're committed to the relationship and to looking after yourself.
Relapse prevention isn't about trying to avoid stress entirely—that's just not possible. It's about building the awareness to recognise your personal warning signs early and having a clear, pre-planned response to protect your wellbeing.
This awareness is your greatest asset in building a more resilient, healthier life.
Creating Your Personal Wellness and Relapse Prevention Plan
A vital part of long-term recovery is becoming an expert on you. This means learning to spot the subtle signs that your stress levels are creeping up, long before you get anywhere near a crisis point. These are your unique early warning signs.
They might include:
Physical signs: Tension headaches, an upset stomach, or finding you’re clenching your jaw.
Emotional signs: Feeling unusually irritable, weepy, or just emotionally numb.
Behavioural signs: Withdrawing from friends, struggling with sleep, or falling back on unhealthy coping habits.
Once you know your signs, you can create a simple action plan. For example: "When I notice I’m skipping meals and feeling constantly irritable, I will take a day off work, go for a long walk, and call my therapist." This proactive approach is incredibly empowering.
It’s especially important because getting professional help isn’t always quick. Recent analysis shows significant delays in UK mental health services, with 16,522 people waiting over 18 months for treatment. Such long waits can increase the risk of relapse, which makes having your own prevention plan absolutely vital. You can read the full analysis on mental health waiting times here.
By designing a life that respects your limits, you move from just recovering to actively building a future where you can genuinely thrive.
Authored by: Therapy-with-Ben
Common Questions About Nervous Breakdown Recovery

The road to recovery is often filled with questions. It's completely natural to have doubts and wonder what the future holds after going through something so intense. I find these are the questions that come up most often in my therapy practice, and I wanted to answer them here to offer some reassurance.
My hope is that having clear, honest answers helps you feel more grounded and empowered. Know that you are on the right track, even when it doesn't feel like it.
How Long Does Recovery Take?
This is probably the number one question I get asked, and the honest answer is: there's no set timeline. It’s a deeply personal journey. How long it takes can depend on the severity of the crisis, what kind of support you have around you, and the underlying reasons that led to the breakdown in the first place.
Some people feel a significant shift within a few months. For others, it’s a year or more of gradual, steady progress.
The most important thing to remember is that the goal is sustainable healing, not speed. I’ve seen time and again that trying to rush the process can set you back. As much of the NHS data suggests, the journey to feeling fully yourself again is often a longer-term one, and that's okay.
Recovery is not a linear path with a set destination. It is a gradual unfolding, with good days and tougher ones. The aim is not to get back to who you were, but to move forward into who you are becoming.
Will I Have to Take Medication Forever?
Not necessarily. Medication can be an incredibly helpful tool, especially in the early stages of recovery. It can help stabilise your mood and quieten those overwhelming symptoms, giving you the headspace you need to properly engage with therapy and learn new ways of coping.
I've worked with many clients who, under the careful guidance of their GP or a psychiatrist, have been able to taper off their medication. This usually happens once they feel more stable and have built up a solid toolkit of strategies for managing their mental health. It’s always a personal decision, made in partnership with your healthcare provider, based on your own progress.
How Do I Explain This to My Employer or Family?
Deciding who to tell and what to say is entirely your call. You are in control of your own story, and you only need to share what feels comfortable and safe for you.
Here are a few ways you could approach it:
With your employer: You can keep it simple and say you’re taking time off for a "medical issue." If you need adjustments when you go back, you could explain that you’re recovering from a period of "severe stress and burnout." You don't owe them the full details.
With family and friends: You might feel you can be more open. It could be as straightforward as explaining that you felt completely overwhelmed and needed to step back to focus on your mental and emotional health.
My advice is to prepare a short, simple explanation that feels right for you. The key is to protect your energy by setting boundaries, allowing you to focus on the vital work of healing.
At Therapy with Ben, I offer a supportive, non-judgemental space to explore these questions and navigate your recovery journey. Whether through online sessions or walk-and-talk therapy in Cheltenham, we can work together to build a more resilient future. Find out more at https://www.therapy-with-ben.co.uk.









Comments