Social anxiety disorder NHS: Your Complete Guide
- Therapy-with-Ben
- 3 days ago
- 17 min read
Author: Therapy-with-Ben
Figuring out how to get help for social anxiety on the NHS can feel like trying to solve a puzzle. It’s a big system, and it's not always clear where to start. But taking that first step is a huge act of courage, and knowing what to expect can make all the difference.
This guide is here to be your roadmap. We’ll walk through everything together, from spotting the signs of social anxiety to actually getting treatment, so you feel a bit more in control of the journey ahead.
Understanding Social Anxiety in the UK

Social anxiety is so much more than just being a bit shy or getting nervous before a big presentation. It's a deep, persistent fear of being watched and judged by others, and it can turn everyday situations into sources of real dread.
Think of it like having a constant internal critic, replaying every conversation on a loop, pointing out every tiny mistake you think you made. Or that gut-wrenching feeling of panic before you even leave the house. For many people, this is a daily reality that chips away at their work life, relationships, and overall well-being.
The most important thing to realise is that you are not on your own with this. Social anxiety disorder (SAD), sometimes called social phobia, is one of the most common mental health conditions in the UK, even if it's not always talked about. Lifetime prevalence rates can be as high as 12%, which actually makes it more common than other conditions like generalised anxiety disorder (which sits around 6%).
Moving Beyond the Clinical Definition
To really get what it’s like, we have to look past the textbook definitions and see how social anxiety shows up in real life. It’s not just about a fear of public speaking; it’s about things like:
The physical dread you feel before a simple work meeting or making a phone call.
The sheer exhaustion that comes from trying to act "normal" and hide your anxiety in social settings.
Actively avoiding things other people take for granted, like parties, eating in a restaurant, or even just popping to the shops.
At its heart, social anxiety is often driven by a powerful inner critic that blows your perceived flaws way out of proportion and convinces you that social failure is inevitable. This voice can be so persuasive that avoiding people feels like the only safe choice, locking you into a cycle that’s incredibly tough to break on your own.
This guide is all about understanding that cycle and finding a way out. We’ll explore the official social anxiety disorder NHS pathways, from that first chat with your GP to the different kinds of therapy available. And while the NHS offers crucial support, we'll also look at other avenues, like finding a local counsellor right here in Cheltenham who might be the perfect fit for you.
Your experience is valid, and with the right support, things can absolutely get better. For some more practical tips, you might find my guide on living with an anxiety disorder helpful.
Recognising the Signs of Social Anxiety

The first step in understanding social anxiety is learning to recognise how it actually shows up in day-to-day life. This is so much more than just being a bit shy; it’s an intense, persistent fear of social situations that can make its presence felt physically, mentally, and in the way you behave.
Often, these symptoms tangle together and feed off each other, creating a cycle that’s incredibly difficult to break. Imagine you’re worried about blushing during a team meeting (that’s a physical symptom). This can trigger a cascade of thoughts about what everyone else is thinking (the mental part), which then makes you want to call in sick for the next one (the behavioural part).
By looking at these signs through the lens of real-life scenarios, you can start to connect the dots with your own experiences. This kind of self-awareness is a huge first step towards getting the right support, like exploring the social anxiety disorder NHS treatment options.
The Physical Feelings of Social Anxiety
Long before your conscious mind has even had a chance to process a social threat, your body is already reacting. It’s that classic 'fight or flight' response kicking in, but instead of being triggered by a genuine danger, it’s set off by something like a party or having to make small talk.
This biological alarm system can feel completely overwhelming. You might be hit with a sudden wave of intense physical sensations that make it almost impossible to think straight or act "normal".
Here are some common physical signs:
A racing heart or palpitations: It can genuinely feel like your heart is trying to hammer its way out of your chest. It helps to understand how anxiety can cause heart palpitations as it's such a common (and scary) symptom.
Blushing, sweating, or trembling: These are particularly cruel because they’re visible. The fear of people noticing them just adds another layer of anxiety to the whole experience.
Shortness of breath or feeling dizzy: You might feel light-headed or like you just can't get enough air in, which can be pretty frightening in its own right.
An upset stomach or nausea: The link between our gut and our brain is incredibly strong, so it's no surprise that social stress can tie your stomach in knots.
These aren't just "in your head"; they are very real, physiological reactions to what your brain perceives as social danger. They’re what can make a feared situation feel genuinely unbearable.
The Cognitive Spiral of Anxious Thoughts
Beyond the physical storm, social anxiety is really defined by a particular pattern of negative thinking. This relentless inner critic often pipes up long before a social event, chatters away throughout, and can stick around for hours or even days afterwards.
Think about it this way: you get an invitation to a colleague's leaving drinks. Your anxious mind might immediately jump to conclusions – you’ll say something stupid, no one will talk to you, you’ll just stand there looking awkward. Then, during the event itself, you might interpret a totally neutral facial expression as proof that someone dislikes you.
The real hallmark of social anxiety, though, is the "post-mortem". This is when you get home and replay every single interaction, picking it apart and criticising yourself for everything you said and did. You become your own harshest judge, utterly convinced you failed.
These thought patterns often feel automatic and completely true in the moment. At their heart is almost always a deep-seated fear of being negatively judged – that you'll be scrutinised, found wanting, and ultimately rejected.
Behavioural Changes and Avoidance Tactics
When you combine those intense physical feelings with such overwhelming negative thoughts, it naturally leads to one thing: avoidance. This is the key behaviour that keeps social anxiety going.
Avoidance isn't always as dramatic as refusing to leave the house. It can be subtle. It might be choosing to send an email instead of picking up the phone, or turning down a promotion because the new role involves managing a team and running meetings.
Other common avoidance tactics include:
Ducking out of social events early.
Using alcohol to "loosen up" and feel more comfortable.
Hugging the walls in a room to avoid being noticed.
Mentally rehearsing conversations again and again.
The problem is, while these behaviours offer a bit of relief in the short term, they end up reinforcing the core belief that social situations are dangerous. This just strengthens the cycle of fear, making it even harder to face those situations next time and causing real disruption to your life.
How to Talk to Your GP About Social Anxiety
The very idea of talking to your GP about social anxiety can feel like a cruel joke. The thing that’s stopping you from living your life is the exact thing you have to face just to get help. It’s a classic catch-22, and it’s completely understandable to feel daunted.
But here’s the thing: this conversation is often the first real step towards getting proper social anxiety disorder NHS support. A little bit of prep can make all the difference, turning a moment of dread into a moment of empowerment.
Remember, GPs talk about mental health every single day. They’ve heard it all before, and they're there to help, not to judge. They know it takes a huge amount of courage to even be in that room. By thinking through what you want to say, you can walk in feeling more in control and ready to get your point across.
Preparing for Your Appointment
You don’t need a perfectly rehearsed speech, but having a few notes scribbled down can be a game-changer. It stops you from getting home and kicking yourself for forgetting something crucial.
Try to jot down some specific examples of how social anxiety is getting in your way. Instead of just saying, "I feel anxious around people," think about the real-world impact.
Here are a few things to consider noting down:
What are your main symptoms? Think about the physical side (that racing heart, blushing, or feeling sick), the internal thoughts (the fear of being judged, worrying you'll say something stupid), and the things you do to cope (like dodging work meetings, cancelling plans, or leaving parties early).
How is it affecting your life? Be honest about the consequences. Has it held you back at work? Is it putting a strain on your friendships or relationships? Do you dread simple things like going to the supermarket?
When did it start and how often does it happen? Have you felt this way for months, or years? Is it a constant feeling, or does it flare up in specific situations? This background info is really useful for your doctor.
Think of your notes as a safety net. If you get overwhelmed or your mind goes blank, you can just look at what you’ve written. It means you’ll say everything you wanted to, even if the anxiety makes it tough to find the words.
What to Expect During the Consultation
In this first chat, your GP’s main job is just to listen and get a clear picture of what’s been going on. They'll likely ask you some questions to understand your symptoms and how they're impacting your day-to-day life.
Don't be surprised if they ask you to fill out a short questionnaire, like the GAD-7 (which is for general anxiety) or one designed specifically for social phobia. This is just a standard way for them to get a more formal measure of what you're experiencing. Just be as honest as you can.
Once they've listened and assessed things, they’ll talk you through the next steps. Most of the time, this will involve a referral to your local NHS Talking Therapies service (you might still hear it being called by its old name, IAPT). They’ll explain what that is and how the referral will work. This is your chance to ask anything you're unsure about, so don't hesitate to ask for clarification if something doesn't make sense.
Your Guide to NHS Treatment Pathways
So, you’ve taken that big first step and spoken to your GP. They’ve agreed a referral is the right way forward. But what actually happens next? This is where you officially enter the social anxiety disorder NHS treatment system, and honestly, it can feel a bit daunting at first.
The key thing to know is that the NHS uses what’s called a "stepped-care" model. Think of it like a ladder. You'll usually start on the first rung with the least intensive, but still effective, treatment. If that doesn't quite get you where you need to be, you can then be "stepped up" to the next rung for something more hands-on. It’s a sensible approach designed to get the right level of support to the right people, without overwhelming the system.
For most people, the first port of call will be a referral to your local NHS Talking Therapies service. You might still hear it called by its old name, IAPT (Improving Access to Psychological Therapies). This is the main hub for proven psychological treatments for common issues like social anxiety.
This flowchart gives you a simple visual of how the journey usually begins.
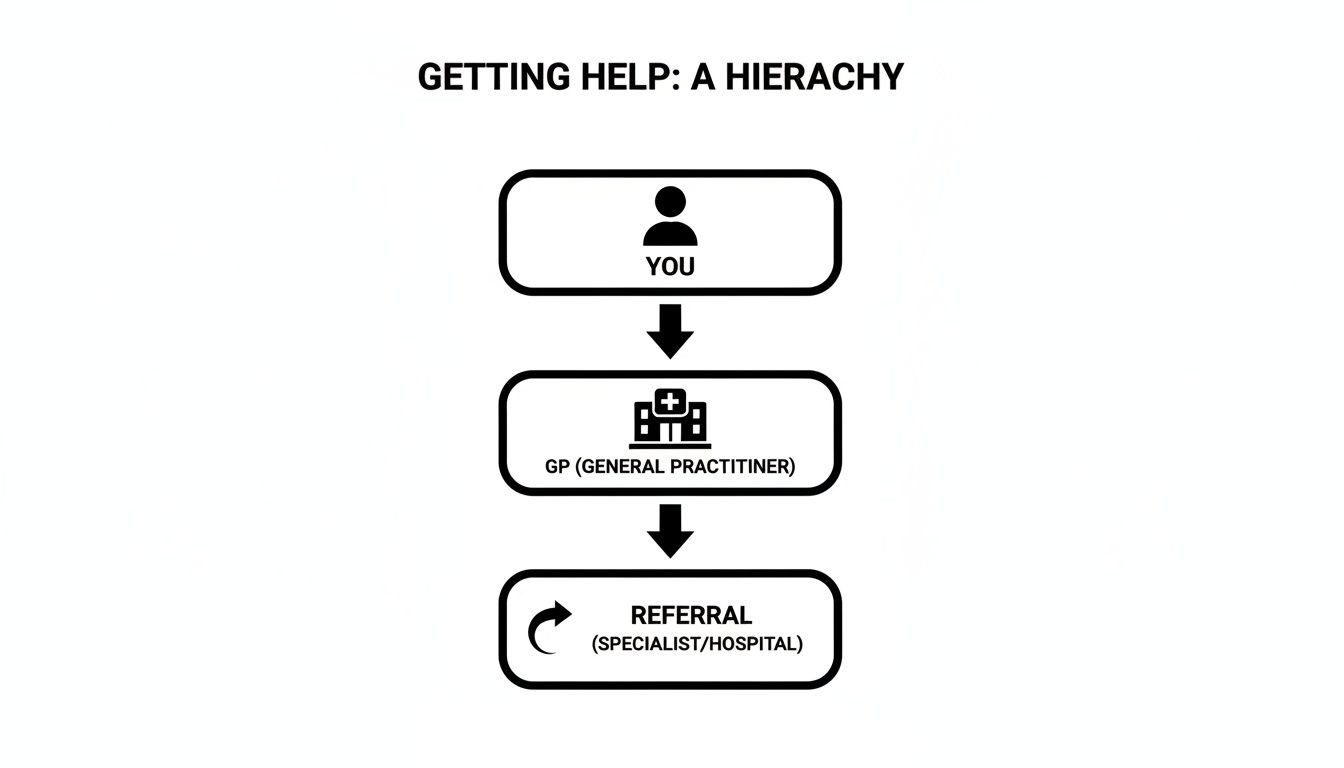
It really is that linear: acknowledging you need help, speaking to your GP, and getting that professional referral sorted.
Cognitive Behavioural Therapy: The Go-To Treatment
When it comes to social anxiety, the gold-standard treatment recommended by the National Institute for Health and Care Excellence (NICE) is Cognitive Behavioural Therapy (CBT). It’s a very practical, structured, and down-to-earth kind of therapy that focuses squarely on the here and now.
CBT is built on a simple but incredibly powerful idea: your thoughts, feelings, physical sensations, and actions are all tangled up together. One can easily trigger the others, trapping you in a vicious cycle.
For instance, you might have the thought, "Everyone in this room is judging me." This thought sparks a feeling of intense anxiety, which then causes physical sensations like a racing heart or blushing. In response, you take action: you stay quiet, avoid eye contact, and leave as soon as you can. CBT helps you unpick that cycle.
Your therapist will work with you to spot these unhelpful thought patterns and gently challenge them. It's not just about talking; you'll be learning practical skills to manage your anxiety in real life.
A typical course of CBT on the NHS often looks like this:
Weekly Sessions: Usually one session a week, lasting about 50 minutes, for a set period—often between 12 and 20 weeks.
Active Work: You’ll be expected to do things between sessions. This might be keeping a diary of your thoughts or trying out small ‘behavioural experiments’ to test your anxious predictions.
Clear Goals: Right at the start, you and your therapist will work out what you want to achieve. This could be anything from speaking up in a team meeting to feeling able to go to a friend’s party.
It's a common misconception that CBT is just about "thinking positively." It's not. It’s about developing a more balanced and realistic perspective, giving you the tools to finally stand up to that harsh inner critic that social anxiety thrives on.
What Else Does The NHS Offer?
While CBT is the main treatment, it isn’t the only one. Depending on your situation and what your local Talking Therapies service can provide, you might be offered a few other options.
Before we dive into those, here’s a quick table summarising the main NHS treatments you’re likely to encounter.
NHS Treatment Options For Social Anxiety Disorder
Treatment Type | What It Involves | Best Suited For |
|---|---|---|
Cognitive Behavioural Therapy (CBT) | One-to-one talking therapy focusing on changing negative thought patterns and behaviours. | People with moderate to severe social anxiety who are ready to actively work on their challenges. |
Guided Self-Help | Working through CBT-based books or online courses with occasional support from a practitioner. | Milder cases of social anxiety, or as a helpful first step while waiting for more intensive therapy. |
Group Therapy | CBT delivered in a group setting with others who have similar experiences with social anxiety. | Those who could benefit from a supportive peer environment and practising skills in a safe social context. |
Medication (SSRIs) | A course of antidepressants, usually Selective Serotonin Reuptake Inhibitors (SSRIs). | People with more severe symptoms, often recommended alongside a talking therapy for best results. |
Each of these pathways offers a different level of support, making sure the care you get is tailored to your needs.
Guided Self-Help
This is often the very first step on the NHS 'ladder'. You’ll be given high-quality, CBT-based resources to work through in your own time – this could be a workbook, a set of online modules, or a recommended book. You aren't left completely on your own, though; you'll have regular, brief check-ins with a therapist or psychological wellbeing practitioner (usually over the phone) to offer guidance and keep you motivated.
Group Therapy
I know, the idea of group therapy can sound like a nightmare for someone with social anxiety. But stick with me here, because it can be unbelievably helpful. It provides a managed, safe space where you can practise your social skills with people who genuinely get it because they’re going through it too. That feeling of realising you’re not the only one is incredibly powerful.
Medication
Medication can also be a really effective tool, especially if your symptoms are quite severe. The most common type prescribed is a Selective Serotonin Reuptake Inhibitor (SSRI). These aren’t ‘happy pills’; they work over several weeks to help regulate your mood and take the edge off the intense physical feelings of anxiety, making it easier to engage with therapy. NICE guidelines typically suggest medication is used with talking therapy, not instead of it.
For a more detailed look at the different ways to find a therapist, our guide on how to get therapy in the UK is a great resource.
Managing NHS Waiting Times with Self-Help Strategies
Getting a referral for therapy is a huge step, but what often comes next is... waiting. Finding yourself on an NHS waiting list can feel incredibly disheartening, especially after you've summoned the courage to ask for help in the first place. It’s easy to feel like you've hit a brick wall before you’ve even started.
But this waiting period doesn't have to be a frustrating limbo. Think of it instead as an empowering head start on your recovery journey. It's a genuine opportunity to begin understanding your anxiety, building some foundational skills, and taking back a sense of control while you wait for formal therapy to begin.
Taking Control While You Wait
Using this time well can make a massive difference. When you start exploring evidence-based self-help techniques, you’re not just killing time; you're laying the groundwork for more effective treatment down the line. These strategies can help you begin to gently loosen the grip that social anxiety disorder NHS guidelines also recognise can be treated.
Many of the skills you'll learn in therapy, especially in CBT, can be introduced at home. This means that by the time your first official session comes around, you’ll already be one step ahead, with a clearer idea of what you want to focus on.
Here are a few powerful, evidence-based strategies you can start with today:
Mindfulness and Grounding: Try some simple mindfulness exercises to pull yourself into the present moment. This is brilliant for quieting the anxious chatter about past slip-ups or future worries. Simple things, like focusing on your breath or the feeling of your feet on the floor, can be surprisingly powerful.
Challenging Anxious Thoughts: Start paying attention to the negative stories you tell yourself about social situations. Ask yourself: "Is there any real evidence for this thought?" or "What's a more realistic way to see this?" This is a cornerstone of CBT, and you can get a deeper understanding by exploring our guide to conquering social anxiety with CBT.
Graded Exposure: This is all about gently and gradually facing the situations you fear, starting with something that feels just a tiny bit scary. If making phone calls is your nightmare, maybe the first step is just calling an automated service. The whole point is to build confidence one small, manageable step at a time.
Waiting for NHS services can feel like being stuck in limbo, but it's crucial to see this period as an active phase of your recovery. By engaging with self-help, you shift from being a passive patient to an active participant in your own wellbeing.
Understanding The Broader Context
It helps to know you’re not alone and to recognise the scale of anxiety in the UK, which goes some way to explaining the pressure on services. In 2022/23, an average of 37.1% of women and 29.9% of men reported high levels of anxiety. While this shows different patterns in who reports it, NICE guidance is clear that social anxiety is common across all genders. Comorbidity—having more than one condition—is also a big factor, with 19% of those with the disorder also experiencing depression.
While you're waiting for formal NHS treatment, these self-help strategies are invaluable. Learning to believe in your own ability to cope can make a huge difference to your recovery. For some practical advice on building that self-belief, guides like How to Build Children's Confidence can offer useful insights.
Starting this work now is empowering. It turns a period of waiting into a time of real, meaningful personal growth.
Exploring Alternatives and Additional Support
While the NHS offers a clear and valuable path for treating social anxiety, it's good to know it's not the only road to feeling better. Sometimes the long waiting lists or the specific therapies on offer might not feel like the right fit for you right now. Looking into other options can put you back in the driver's seat, helping you find support that feels more personal and immediate.
Private therapy is one of the most common alternatives. Its biggest advantage is often speed; you can usually bypass the long NHS waiting lists and be speaking to a therapist within a week or two. When you're really struggling, getting that support sooner rather than later can make a world of difference.
Going private also gives you far more choice. You have the freedom to find a therapist who specialises in social anxiety and choose a therapeutic approach that really clicks with you, whether that's a traditional talking therapy or something a bit different.
Finding the Right Therapeutic Fit
Not all therapy has to happen in a formal office setting. For many people, the very idea of sitting face-to-face with a stranger in a clinical room can feel incredibly intense and just add to the anxiety they're already feeling.
This is where different approaches, like the walk-and-talk therapy I offer here in Cheltenham, can be a real game-changer.
This less formal style of therapy often feels more natural and less confrontational. The simple act of walking side-by-side in a park or along a quiet path can ease the pressure of constant eye contact, making it much easier to open up. It neatly combines the mental benefits of therapy with the physical and psychological boost of being out in nature and moving your body.
Here’s why it works so well for social anxiety in particular:
Reduced Intensity: The environment is relaxed and informal, a world away from a stuffy therapy room.
Natural Conversation: Walking together encourages a more conversational flow, which can feel less like an interrogation.
Physical Release: Gentle physical activity is a proven way to dial down anxiety and stress levels.
The Wider Support Ecosystem
Beyond one-to-one therapy, there's a fantastic network of support available from respected UK mental health charities. These organisations are a goldmine of information, community support, and practical advice that can be a brilliant addition to any formal treatment you receive.
Tapping into these resources is a powerful reminder that you're not on your own with this. They offer a sense of community and understanding that can be a real antidote to the isolation that so often goes hand-in-hand with social anxiety.
Connecting with a charity or a support group reminds you that countless others share your experience. This shared understanding can be incredibly validating and helps to normalise your feelings, reducing the shame that social anxiety often thrives on.
Some of the most well-regarded organisations in the UK include:
Mind: A leading charity offering extensive information on all aspects of mental health, along with a supportive online community and a confidential Infoline.
Anxiety UK: A charity run by and for people with anxiety, they provide a range of services including access to reduced-cost therapy, a helpline, and self-help resources.
These charities act as a vital safety net, offering reliable information and a helping hand whenever you need it. Exploring these alternatives—from private therapy that’s just right for you to the community offered by charities—gives you a whole toolkit for recovery. It ensures you have a broad spectrum of support, allowing you to build a path forward that feels right for you.
Your Questions Answered
When you’re thinking about getting support, it's natural for a load of questions to pop up. Let’s tackle some of the most common ones that I hear, hopefully giving you a bit more clarity as you consider getting help for social anxiety disorder NHS services.
Can I Choose My Therapy on the NHS?
This is a really common question. The NHS generally uses what's called a 'stepped-care' approach. Think of it like a ladder – you start on the first rung with the most straightforward, effective treatment, which might be guided self-help or group CBT.
You absolutely can, and should, chat with your GP or therapist about what you think might work best for you. Your voice matters. However, the final decision often comes down to a clinical assessment of your needs and, frankly, what's available in your local area. It never hurts to ask, though.
Will the NHS Give Me Medication for Social Anxiety?
Yes, medication is definitely an option and can be a big help, especially when it's combined with talking therapy. The go-to medications for anxiety are usually a type of antidepressant called Selective Serotonin Reuptake Inhibitors (SSRIs).
Your GP is the best person to talk to about whether this route is right for you. It’s worth knowing that the official guidelines from the National Institute for Health and Care Excellence (NICE) suggest that medication works best alongside a psychological therapy like CBT, rather than just on its own.
What if I Have a Panic Attack When I'm Out?
Panic attacks feel awful, and they're a very real and distressing part of social anxiety for many people. If you feel one coming on, the first step is to try and find a quieter spot if you can, even if it's just turning to face a wall for a moment. Then, bring all your attention to your breath – a slow breath in, and an even slower one out.
A great tool in the moment is grounding. Try to name five things you can see, four things you can touch, and three things you can hear. This simple act can pull your mind back from the brink. The most important thing to remember is that a panic attack, as terrifying as it feels, isn't dangerous and it will end. Therapy is brilliant for building up your own toolkit to manage these moments.
How Is Social Anxiety Different from Autism?
This is a fantastic and important question. While on the surface they can look similar because both can involve finding social situations tough, the reasons behind it are quite different. Social anxiety is fundamentally a fear – a fear of being judged or embarrassing yourself.
For an autistic person, social difficulties are more often about differences in how they process the world, communicate, and handle sensory information. It's also very common for an autistic person to also have social anxiety, because trying to navigate a world not built for you can be incredibly stressful. A proper assessment can help figure out what’s going on so you get support that actually fits.
At Therapy-with-Ben, I offer a compassionate and understanding space to explore these challenges, including specialised walk-and-talk therapy in Cheltenham. If you feel ready to take the next step beyond the NHS or want to explore your options sooner, please get in touch. Find out more at https://www.therapy-with-ben.co.uk.








Comments